 As we know, the law requires that a medical benefit which includes, but is not limited to, the treatment, a device or an aid be medically necessary. In order to award that benefit, the test is whether it is medically necessary. A Judge of Compensation Claims may award only those medical benefits that are medically necessary. It is important to understand the distinction between a medically necessary benefit and those that are merely pleasant or convenient. Simple convenience will not suffice nor would a benefit that would neither improve nor aid in recovery be considered medically necessary.
As we know, the law requires that a medical benefit which includes, but is not limited to, the treatment, a device or an aid be medically necessary. In order to award that benefit, the test is whether it is medically necessary. A Judge of Compensation Claims may award only those medical benefits that are medically necessary. It is important to understand the distinction between a medically necessary benefit and those that are merely pleasant or convenient. Simple convenience will not suffice nor would a benefit that would neither improve nor aid in recovery be considered medically necessary.
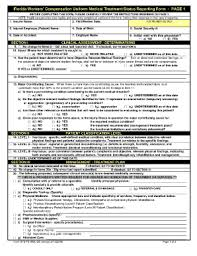
After each doctor visit, the injured worker must obtain a completed DWC 25 – which documents the medical recommendations. The completed DWC 25 along with progress notes will be sent directly to the adjuster for approval or denial. If the adjuster fails to respond within 10 days of receipt, the statute specifically states that medical necessity is waived. See 440.13 (3)(i) (states “a claim for…surgical operations … is not valid and reimbursable unless services have been expressly authorized by the carrier, unless the Carrier has failed to respond within 10 days to a written request for authorization, or unless emergency care is required”.
In the past, the adjusters have argued that the DWC 25 is not enough as progress notes must also be attached making the recommendation for any and all medically necessary treatment. The adjusters are correct!
In a recent case, the judge concluded that the carrier failed to respond to the written request for authorization of the recommended surgery within 10 days of receipt and is therefore required to authorize the procedure, unless there is a showing that the procedure is not within the practice parameters and protocols. See Lomonte v. Target/Sedgwick CMS, OJCC 11-013660MGK
The judge further concluded that the DWC 25 without the associated progress note is not enough to start the 10 day clock. Keep in mind, a health care provider is required to submit treatment reports so that an informed decision may be made as to what benefits are to be provided, and those benefits then provided in a timely manner. However, once the progress notes are forwarded to the adjuster, the clock starts.
Ultimately the Judge concluded that the carrier failed to respond to the written request for authorization of the medical procedure within 10 days of receipt and is therefore required to authorize the medical procedure unless there is a showing that the procedure is not within practice parameters and protocols. There was no evidence that the procedure was not within practice parameters and protocols. As such, the surgery was deemed medically necessary and same was granted.
Is your recommended medical treatment medically necessary? For more information, call Joann Hoffman and Associates PA for a free consultation.
 Florida Injury Attorneys Blog
Florida Injury Attorneys Blog


